1.1 Anatomia e Fisiologia do sistema respiratorio

puppies
O principal trabalho dos pulmões é cambio de gas, inserir oxigénio no corpo e se livrar do dioxido de carbono.Normalmente durante uma inalação o diafragma se contrai a puxar para baixo e os musculos do peito se contarem ......
The main job of the lungs is gas exchange, pulling oxygen into the body and getting rid of carbon dioxide. Normally during an inhale the diaphragm contract to pull downward and the chest muscles contract to pull open the chest which both help suck in air like a vacuum and then during an exhale the muscles gets relaxed allowing the lungs to spring back to their normal size which pushes air out.
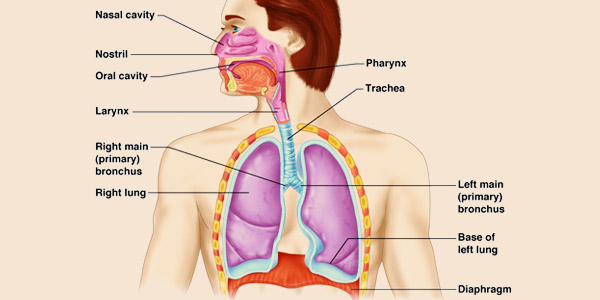
Respiratory System
When you breathe in air flows through the nostrils and enters the nasal cavity which is lined by cells that release mucus. That mucus is salty sticky and has lysozymes which are enzymes that help kill bacteria. Nose hairs at the entrance of the nasal cavity get coated with that mucus and are able to trap large particles of dust and pollen as well as bacteria forming tiny clumps of boogers. The nasal cavity is connected to four sinuses which are air-filled spaces inside the bones that surround the nose called the paranasal sinuses. Maxillary sinus helps the inspired air to circulate for a bit so it has time to get warm and moist. They also act like tiny echo chambers that help amplify the sound of your voice, this is why you sound so different when you plug your nose or if they get clogged with puke astoria cold.
That relatively clean warm and moist air goes from the nasal cavity into the pharynx or throat, the region connecting the two is called the nasal pharynx and the part connecting the pharynx to the oral cavity is called the oropharynx. The soft palate which is the softer portion of the roof of your mouth behind the hard palate which is the part you can feel with your tongue and the pendulum like uvula hanging at its end move together to form a flap or valve that closes the nasal pharynx off when you eat to prevent food from going up into the nasal pharynx.
Finally there's the laryngopharynx the part of the pharynx that's continuous with the larynx or the voice box up to this point. Food and air share a common path but at the top of the larynx it's a spoon shaped flap of cartilage called the epiglottis which acts like a lid that seals off the airway when you're eating so that food can only go one way down the esophagus and towards the stomach. If anything other than air gets into the larynx then you have a cough reflex that kicks it right back out. Now once air makes its way into the larynx it then continues down the trachea or windpipe which splits into two main stem, bronchi, the point at which they split is called the Carina. It then enters the lungs.
The right lung has three lobes, the upper lobe, middle lobe and lower lobe. The left lung just has two lobes the upper lobe and the lower lobe. The right mainstem bronchus is wider and more vertical than the left which is why if you accidentally inhale something big that can't get coughed up like a peanut it's more likely to go into the right lung than the left. The main stem bronchi then divide into smaller and smaller bronchi, the trachea and the first three generations of bronchi are all pretty wide and use cartilage rings for support.
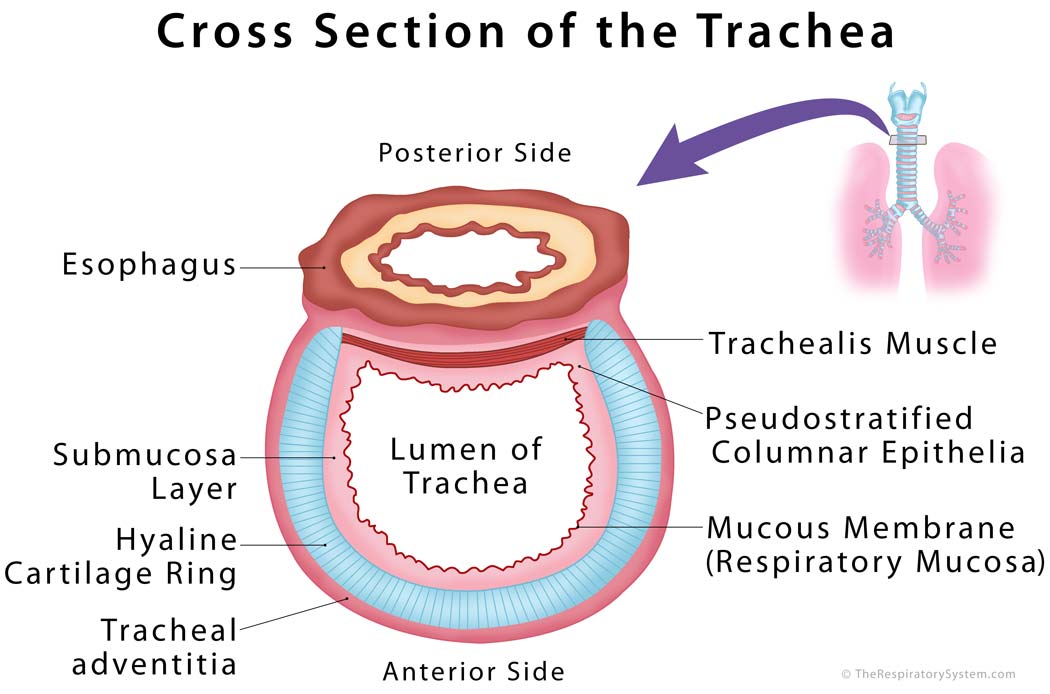
Cross Sectoin of Trochea
Now taking a look at a cross-sectional chunk of this trachea there's also a layer of smooth muscle which has nerves of the autonomic nervous system in it. The autonomic nervous system is made up of two basic types of nerves, sympathetic nerves which are involved in fight-or-flight mode like running from a turkey and parasympathetic nerves, which are involved in the rest and digest mode like eating ice cream on the beach.
Smooth muscle along the trachea and the first few branches of bronchi have beta-2 adrenergic receptors going back to that turkey when you're running the sympathetic nerves stimulate those beta-2 adrenergic receptors and this increases the diameter of the Airways allowing more air to get in but those same Airways also have muscarinic receptors which can get stimulated by parasympathetic nerves causing a decrease in the diameter of the Airways. The large Airways are lined mostly by ciliated columnar cells and a handful of goblet cells which get their name from looking like a wine goblet and these guys secrete mucus. That mucus helps trap particles and then the ciliated columnar cells beat rhythmically to move the mucus and any trapped particles from the air towards the pharynx where they can either be spit out or swallowed. This mechanism is known as the mucociliary escalator.
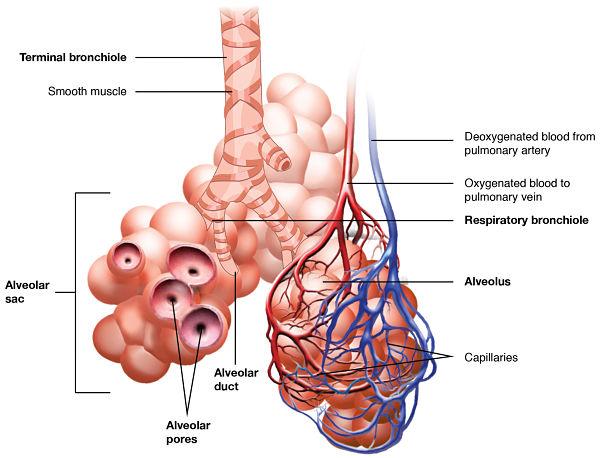
Bronchioles
After the first three generations of bronchi though the airwaves get more narrow called bronchioles meaning little bronchi and these can stay open without the need for cartilage air is conducted through smaller and smaller bronchioles for about 15 to 20 generations and collectively these are known as conducting bronchioles. These conducting bronchioles receive oxygenated blood from the bronchial arteries the walls of those conducting bronchioles are also lined by ciliated columnar cells. In mucus secreting goblet cells as well as a new type of cell called a club cell. These Club cells secrete glycosaminoglycans which protect a bronchial or epithelium, these guys can also transform into ciliated columnar cells so they help regenerate and replace damaged cells, if needed.
Now all these cells the bronchioles receive oxygenated blood from the bronchial arteries of the systemic circulation which is important to keep in mind for later the last part of the conducting bronchioles are the terminal bronchioles and then after that air gets the respiratory bronchioles which are unique because they have tiny outpouching that butt off from their walls these outpouching x' are called alveoli and there are about 500 million of them in the lungs.
Eventually the respiratory bronchioles end when there's nothing but alveoli and at that point the airway is called an LV ler duct rather than a respiratory bronchial and this is the final destination of the inhaled air the alveolar wall has a completely different structure than the bronchioles. There are no cilia or smooth muscle and instead the walls lined by sin epithelial cells called pneumo sites most our regular pneumo sites called type 1 pneumo sites. But some called type 2 pneumo sites have the ability to secrete a substance called surfactant surfactant helps decrease the surface tension within the alveoli and therefore helps keep them open just like the club cells the type to nuuma sites are capable of transforming into type 1 pneumo sites so they can also help regenerate and replace damaged cells.
Finally if a tiny particle ever makes it deep into the lungs there are alveolar macrophages that can gobble it up and then physically move up to the conducting bronchioles where they can ride the mucosal iary escalator all the way up to the pharynx to be either coughed up or swallowed down free from particles the inhaled air is now in the alveolus surrounded by mostly type 1 pneumo sites. On the other side of the numa sites are endothelial cells that line the capillary walls which is what holds the blood this time though that blood comes from the pulmonary arteries and is deoxygenated the pneumo sites and the capillaries are glued together with a protein layer called the basement membrane so the alveolar wall the basement membrane and the capillary wall is really all that separates the air from the blood and this is called the blood gas barrier. At this point carbon dioxide diffuses out from the deoxygenated blood and into the air of the alveoli which then gets breathed out and with each breath in oxygen enters the alveoli and freely diffuses into the blood that's freshly oxygenated blood then heads off to the pulmonary veins the heart and then to the body's tissues.
References
- https://training.seer.cancer.gov/anatomy/respiratory/
- https://www2.estrellamountain.edu/faculty/farabee/biobk/BioBookRESPSYS.html
- https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0022181/
- https://www.brainpop.com/health/bodysystems/respiratorysystem/
About Author
Professor and Head, Department of Anatomy, Senior Lecturer & Consultant Surgeon, Professor-in-Charge, Medical Education Unit at St. Joseph's Hospital and Medical Center, Phoenix, Arizona. Currently working as a content developer of anatomy at Earth's Lab.